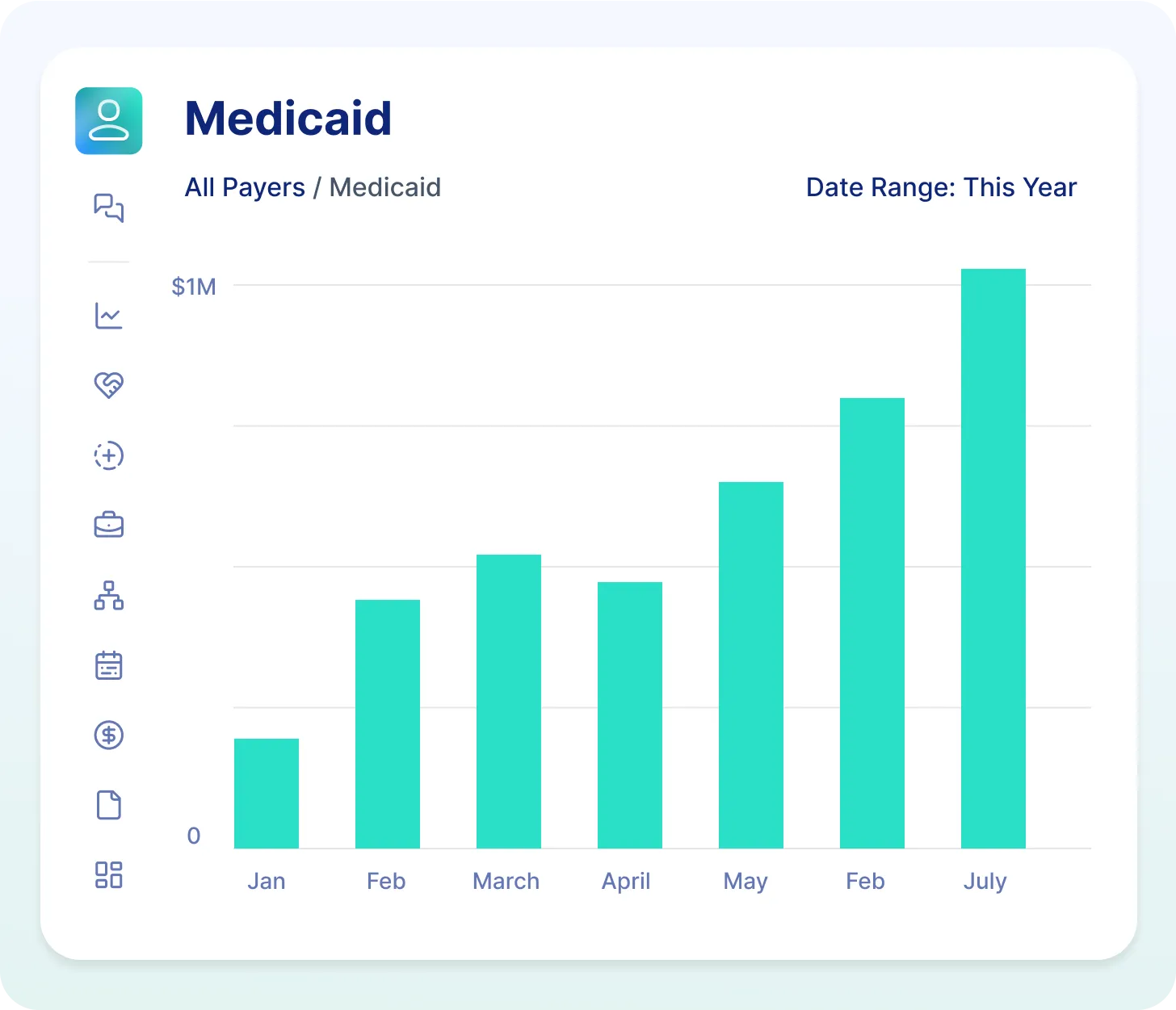
Medicaid Claims Management For Home Care Agencies
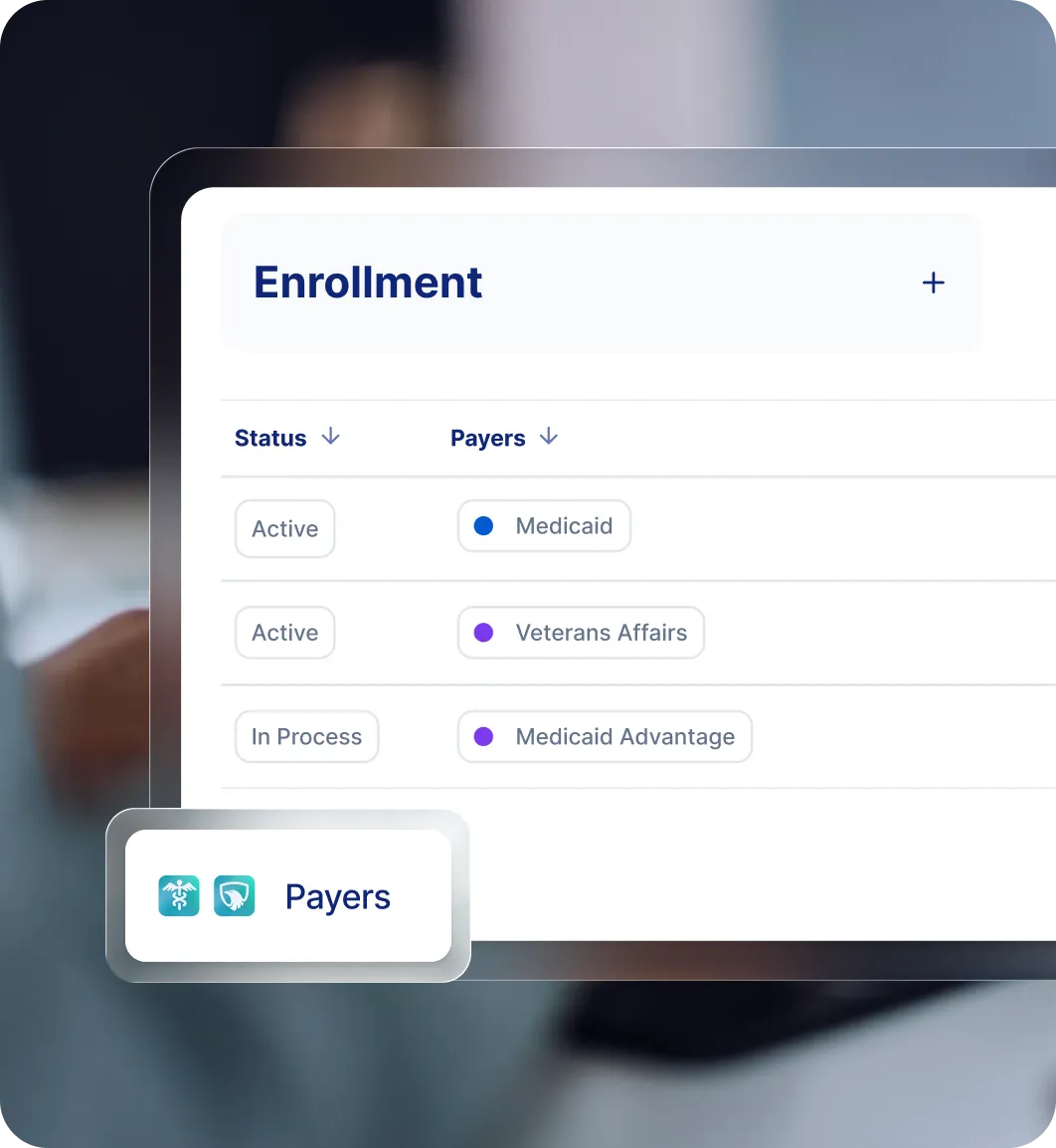
Medicaid can be one of the most reliable payers in home care, but only if your billing, authorizations, and eligibility checks are airtight. Paradigm manages the complexity so you can focus on delivering care and growing your business.
How It Works
We only charge for successful Medicaid claims, so our success depends on yours.
Expert Medicaid billers and AI-powered tools
We run your Medicaid claims like we’re your in-house billing department
.png)

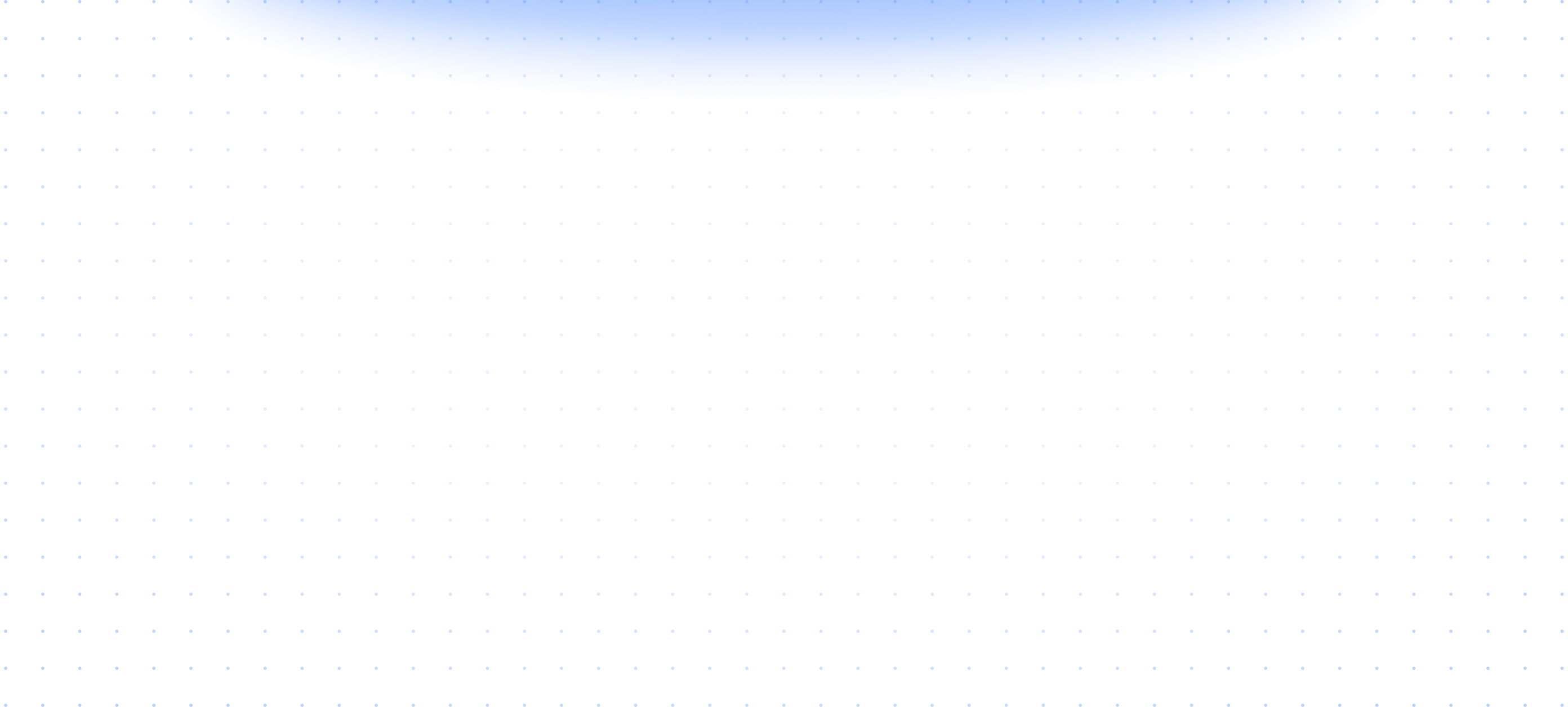
Human touch without human error
Our AI-powered billing tools scrub shifts, check authorizations, and reconcile payments
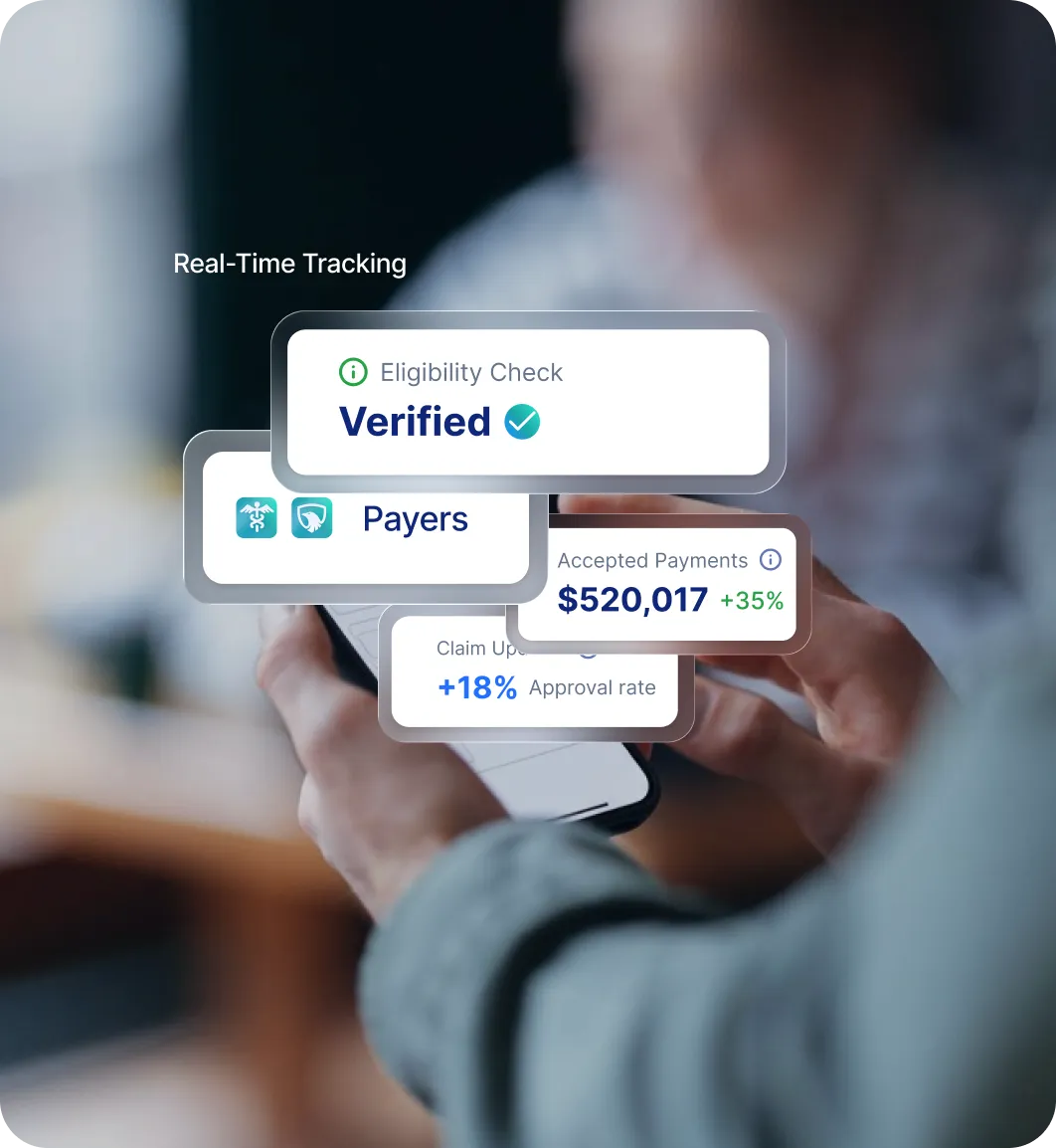
We get you enrolled in Medicaid
We help you get enrolled with state Medicaid programs and MCOs, if you aren’t already
We Take Care Of It All
Partnering with us will feel like you’ve gained a team of coworkers who’ve spent their whole careers mastering Medicaid.

Grow Faster With
Expert Growth Coaching
Our revenue grows with yours, so we provide free growth coaching to our customers. Our veteran coaching team includes former agency owners, franchise trainers, sales coaches, and more.
Grow Faster With
Expert Growth Coaching.
Our growth depends on your growth. So we assembled a team of home care experts to help you out.
The coaching team includes former agency owners, franchise coaches, sales coaches, and more.
Frequently Asked Questions
Can Paradigm help me enroll in Medicaid or with MCOs?
Can Paradigm bill directly in my EVV or agency management system?
What if I’m already doing Medicaid billing but it's a mess?
Do you reconcile EVV with shifts?
How does Paradigm charge for Medicaid billing?
Can you help with both Medicaid and the VA billing?
Do you handle Medicaid claim denials and appeals?
Do you help track Medicaid authorizations?
Does Paradigm provide Medicaid-specific training?

Your bank account deserves More Cashflow.
Got questions about Medicaid billing services? Let’s talk.