Get Paid On Time Without Worrying About It
We don’t just submit VA and Medicaid claims; we manage the entire home care billing cycle, from EVV matching to payment posting, so you don’t have to chase down a dime.

What We Handle
We only bill on successfully paid claims, so our success depends on yours.

VA Billing Software



Medicaid Billing Software



What Makes Our Process Different?
It’s not our first rodeo, or even our 1,000th rodeo. We manage VA and Medicaid billing by proactively running checks on the information most likely to cause denials, escalate appeals rapidly when needed, and maintain relationships with the payers.
Full-Cycle Billing
We don’t stop at submission. We scrub claims, verify all documentation, manage denials, and post payments so your team can stay focused on care.
Platform-Agnostic Integration
We work with most major AMS and EVV systems. Whether you’re using WellSky, HHAeXchange, or something custom, we fit into your workflow.
Smart Shift Scrubbing
Before a claim is submitted, we match each shift against authorizations, EVV, and payer rules. That means fewer rejections and cleaner AR.
Denial Prevention + Follow-Up
Our system flags high-risk claims before they go out—and if something does get denied, we escalate it fast and follow it through to resolution.
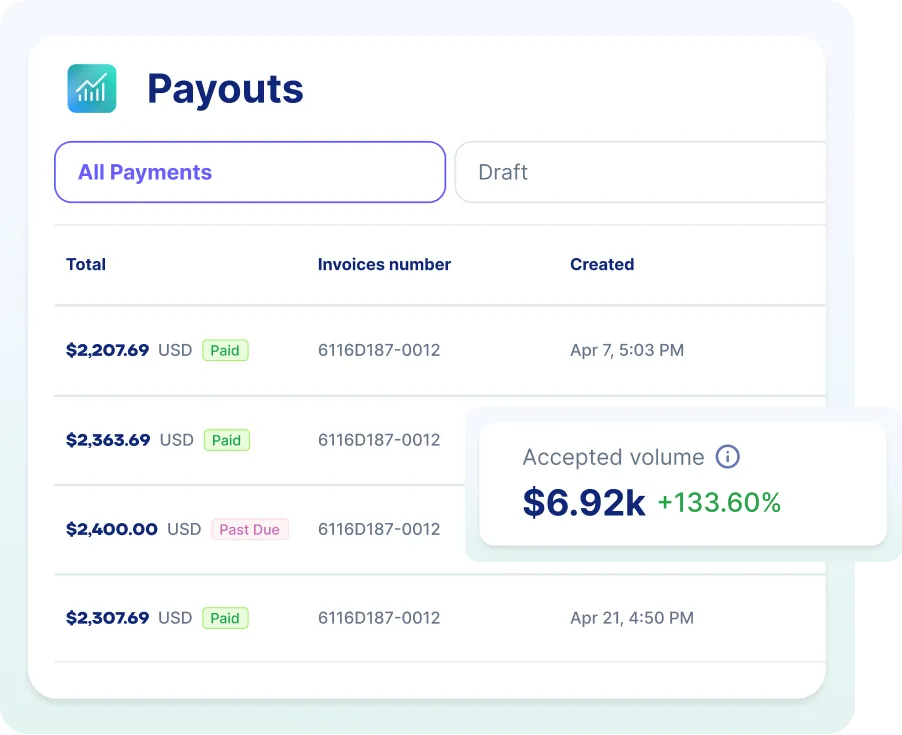
Real-Time Visibility
You’ll always know where things stand. Our portal tracks every claim, every payment, and every unresolved issue. No more guesswork.
Pay-For-Performance
We don’t charge you until you get paid. That means our goals are aligned with yours—and we’re motivated to keep cash flowing.
Frequently Asked Questions
Do I have to use HSRM?
How do I know if a shift is billable?
What if a claim is denied?
Do you reconcile payments?
What gets VA claims rejected?
Which systems do you work with?
Do you submit through clearinghouses?
How do you handle denials?
Do you match EVV and authorizations?
How soon after service do you bill?

Let us do the dirty work
You’ve already done the hard part—delivering care. We’ll make your life easier by ensuring you get paid fully, quickly, and without friction.



