Get rolling In Record Time
Be it Medicaid or VA, we’ll guide you through the red tape and kickstart your home care agency's growth.

What We Handle
We act as hands-on enrollment and credentialing consultants for the VA and Medicaid with a personal stake in getting your home care agency to the billing stage.

VA Credentialing



Medicaid Enrollment




What Makes Our Process Different?
It’s not our first rodeo, or even our 1,000th rodeo. We manage credentialing and enrollment by proactively running checks on the information most likely to cause denials, escalate appeals rapidly when needed, and maintain relationships with the payers.
Strategic market targeting
We help you avoid saturated counties, closed panels, and underfunded waiver programs. You’ll start with a clear, viable path to referrals.
No missed steps
We check everything—NPPES, CAQH, license alignment, liability coverage—before any submission. One missed item can delay your approval by 60+ days.
Full-service submission
We don’t just send you instructions. We complete the forms, handle follow-ups, and coordinate with state and federal contacts until you’re approved.
Credentialing with context
Enrollment decisions affect how you bill later. We ensure your NPI setup, taxonomy, and service listings match billing rules from day one.
Real-time updates
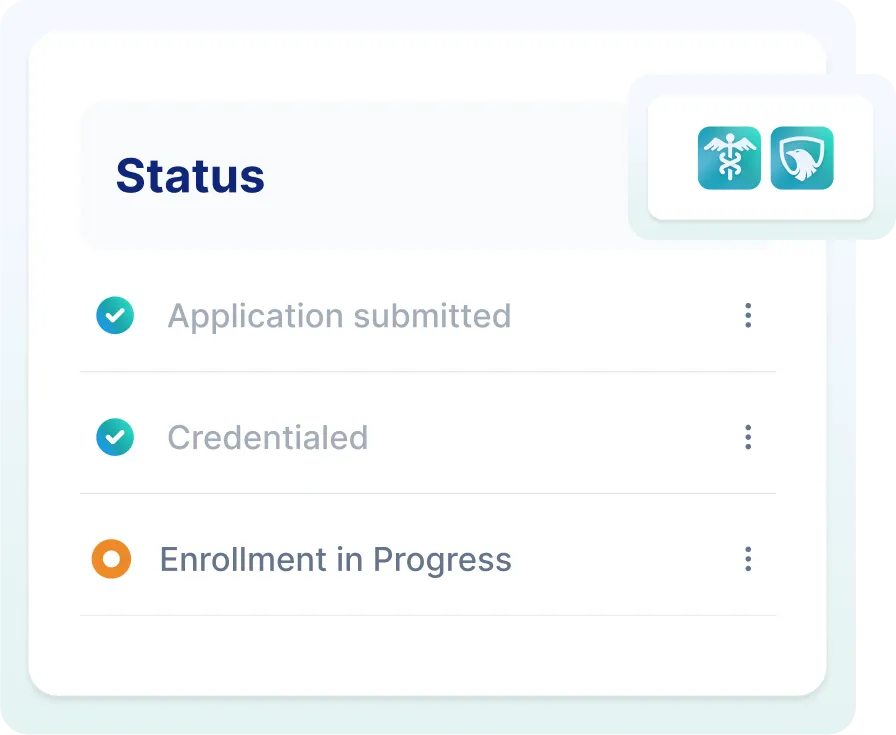
No more wondering if your application is just “sitting somewhere.” Our team and portal give you clear status updates at every step.
Billing-ready onboarding
Once you’re credentialed, you’re ready to bill. We configure everything for a seamless transition to authorizations, EVV, and claims submission.
Frequently Asked Questions
How do I know if I’m eligible for VA billing?
Do you help with both Optum and TriWest?
What documents do I need to provide to the VA?
How long does it take to get approval from the VA?
What if my market is “closed”?
Do you support my state?
What’s included in the enrollment fee?
What if I already started the process?
How long does Medicaid enrollment take?
Which waivers or MCOs will I need?

Let’s Get You Set Up The Right Way
You don’t need a consultant who only knows the paperwork.
You need a credentialing partner who understands how these systems work—and how to get you paid.



